The Shape of Dying: The Four Illness Trajectories
The Shape of Dying
By noon, she was unconscious. But earlier that morning, her mother had eaten three good bites of oatmeal. Every similar quiet breakfast prior had felt like proof she would recover—until that day. The daughter remarked to us, “No one said it could go this fast.”
To relieve suffering, we need to know a little about future. “We can’t predict an exact date of death, but we can trace its path and prepare for what’s likely.”
Doctors often overestimate how long patients will live—sometimes by a factor of five ( Christakis & Lamont, 2000). This can delay hospice signup and leave families unprepared. We speak of “unexpected deaths” in people who are seriously ill, even on hospice. Paradoxically those professionals who know the patient the best are often the worst at prognostication.
Knowledge of basic illness trajectories—Sudden Death, Terminal Illness, Organ Failure, and Frailty—helps you plan. These patterns, described by first in the early 2000s, are maps of future decline.
“Death never arrives unannounced. It simply finds us unprepared.” — adapted from Seneca.
That’s why we ask: “Is this patient likely to live six months or less?” The answer informs hospice eligibility. Another question is the Surprise question: “Would you be ‘shocked’ if this patient were still alive in 12 months?” This framework from UK’s Gold Standards prompts planning over prediction. Use these two questions to think about eligibility broadly. Then consider disease trajectory and how if might advance.
“Trajectory recognition is how we move from hospice eligibility to hospice strategy. It transforms IDG from reactive to prepared.” — Brian H. Black, D.O.
The Four Common Trajectories of Decline
Each broad category of slope carries its own pace and preparation. Imagine four lines on a graph—one drops like a cliff, one plunges after a long plateau, one dips and rises in jagged waves, and one slopes so gently at times you almost miss it.
Visual Reference: The Four Trajectories of Functional Decline
Source: Lunney JR, Lynn J, Hogan C. Patterns of functional decline at the end of life. JAMA. 2003;289(18):2387–92.
This model helps you recognize patterns early. Published in JAMA in 2003, it not only introduced this now-familiar above visual but confirmed clinical relevance with more than 4,000 patients. The study remains a grounded source for hospice trajectory education.
| Trajectory | Condition | What to Expect | How to Prepare |
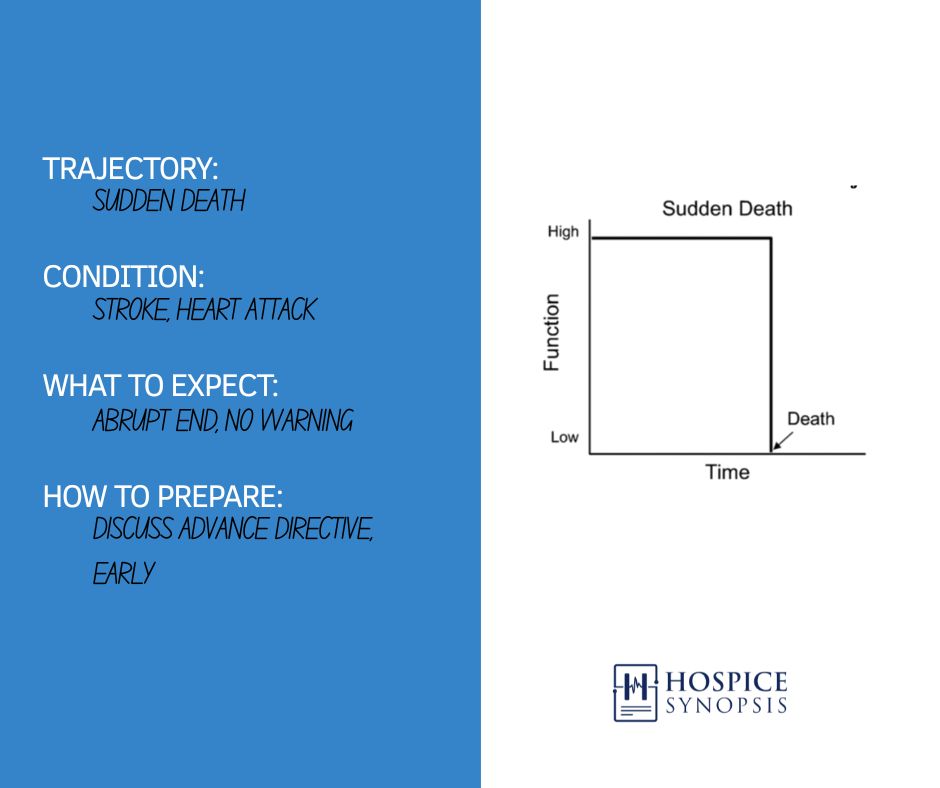
| Sudden Death | Stroke, Heart Attack | Abrupt end, no warning | Discuss Advance Directive Early |
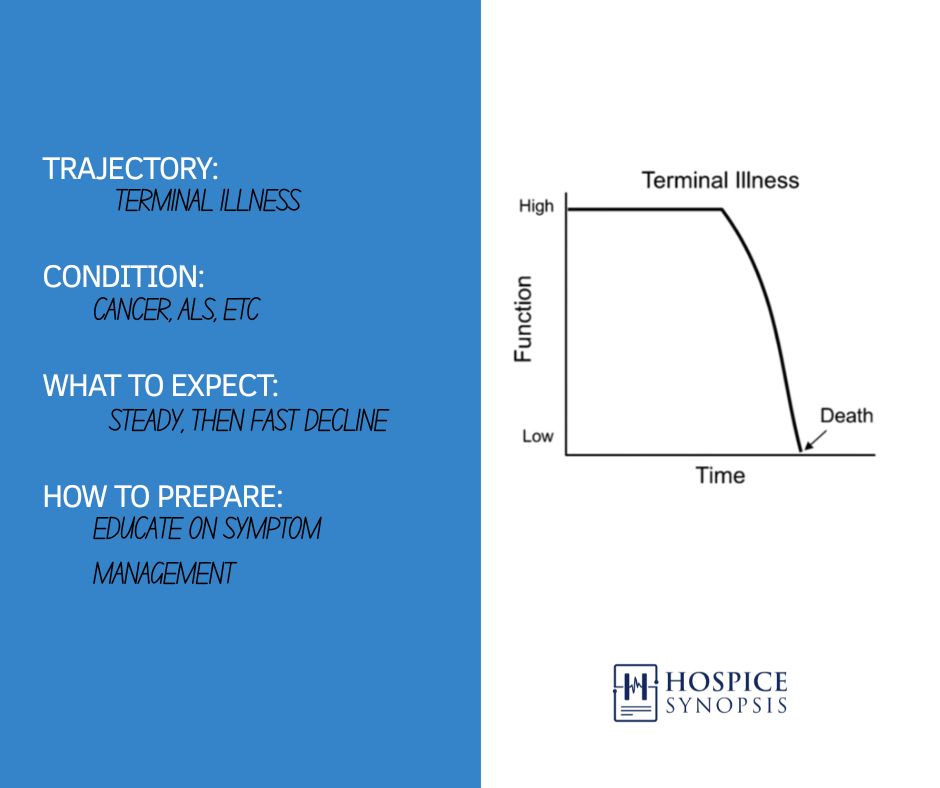
| Terminal Illness | Cancer, ALS | Steady, then fast decline | Educate on Symptom Mgt. |
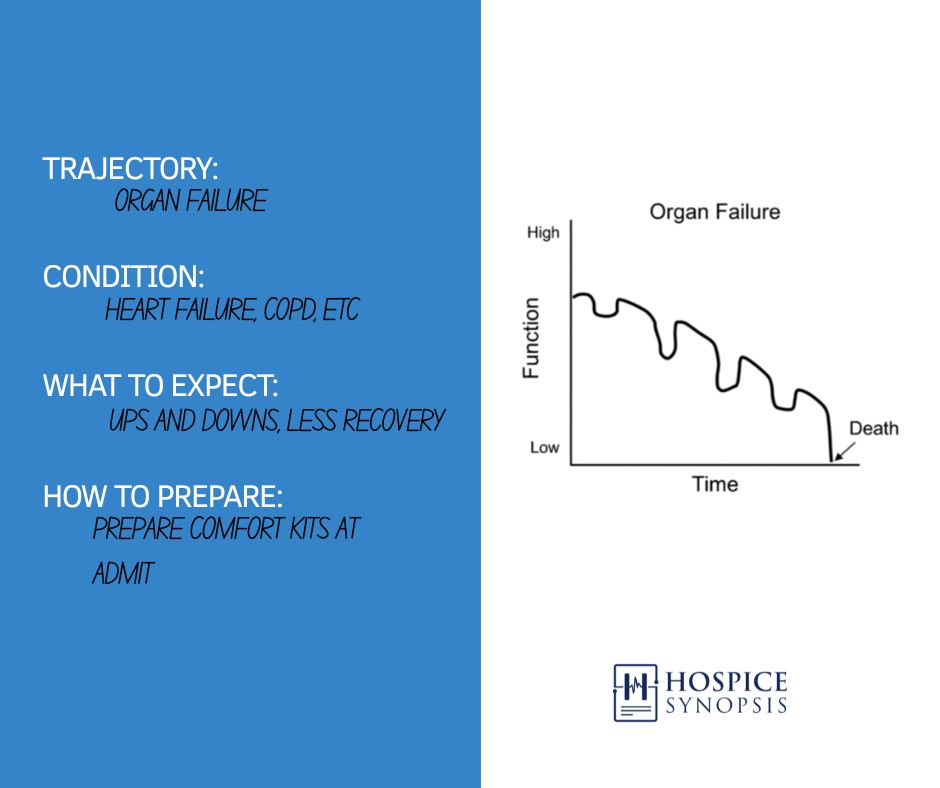
| Organ Failure | Heart Failure, COPD | Ups and downs, less recovery | Prepare Comfort Kits at Admit |
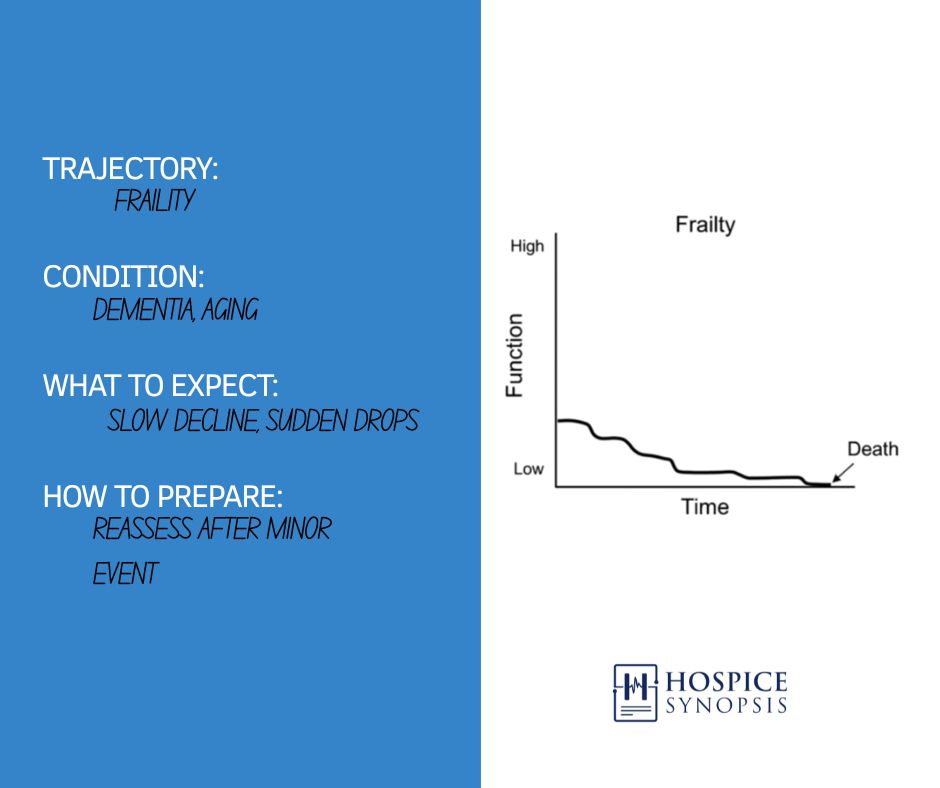
| Frailty/Dementia | Dementia, Aging | Slow decline, sudden drops | Reassess after minor event |
- Sudden Death – High function until abrupt end; often precedes hospice referral.
- Terminal Illness – Stable function with steep decline.
- Organ Failure – Repeated crises, incomplete recoveries.
- Frailty/Dementia – Long, slow decline until a minor event causes collapse.
Prognostication: A Skill Worth Pursuing
Why Prognostication Matters
Families don’t need certainty. They need orientation.
Tools for Better Forecasting
A 2014 study by Paiva and Bruera showed that function and symptom burden predict better than diagnosis alone. The Palliative Performance Scale (PPS), which measures a patient’s ability to perform daily activities, reveals what lab tests can’t always show. While symptom burden, tracked over time, reveals the shape of decline.
Naming the trajectory aligns care with reality. It informs—not replaces—clinical judgment.e. What begins as a misunderstanding often ends as mistrust, just when families are looking for someone to help carry the weight.
The Interdisciplinary Group’s (IDG) Role in Trajectory Recognition
When the Team Misses the Pattern
When the Interdisciplinary Group (IDG), the team of nurses, social workers, aides, and chaplains, fails to name the trajectory:
- The nurse under-forecasts decline.
- The social worker misses anticipatory grief cues.
- The aide’s instincts are ignored.
- The chaplain senses withdrawal but can’t explain it.
- The family is unprepared.
Common Pitfalls
- Over reliance on labs
- Making inferences with limited information
- Hesitating to name a trajectory due to fear of being wrong, thereby delaying preparation.
- Underestimating the observations of experienced staff
When the Team Names It Clearly
- Expectations align.
- Medications make contextual sense.
The team plans for what’s coming—not just what is.
A seasoned social worker said: “When families think they have months and we know it’s days, their grief gets ambushed.”
No single discipline owns trajectory recognition. It’s a shared clinical mosaic, and as a new physician, you’ll rely on your IDG to refine this skill.
Turning Recognition into Action
How to act on a trajectory as a new hospice physician:
- Document it: “Organ failure trajectory, likely more and worse heart failure flare-ups.”
- Say aloud: “This pattern may repeat—with poorer recovery.”
Example: You notice a COPD patient’s recent hospitalization signals an Organ Failure trajectory. Document this in the chart and propose a comfort kit at the next IDG to prepare for worsening crises.
This informs your team and the family, building confidence in your clinical decisions.
First Steps checklist:
- Assess present and historical function with patient, family, and via the clinical records.
- Ask IDG about recent trajectory shifts during reviews.
- Practice the family forecast script in team discussions
- Care Plan and frequently reassess
Mapping Trajectories: From Pattern to Practice
Note: Some patients shift trajectories after new injuries, infections, or weight loss. For example, a COPD patient may follow a frailty-like course after an aspiration event. IDGs should re-map trajectories after major clinical changes.
Steps for Teams
Tip for IDG Chairs: Use a 2-minute teach-in to normalize trajectory talk. “Let’s name the likely trajectory—then check if our care plan matches it.”
Caution: Trajectory slope doesn’t dictate visit frequency, but steeper declines may require rapid plan revisions or urgent physician follow-up.
- During IDG Review
- Identify the primary trajectory.
- Note changes in slope, crises, or recoveries.
- As a Documentation Anchor
- In notes or visits: “Continues on a frailty trajectory with PPS of 40%, minimal reserves. Now a 2-person assist to chair in the last 2 weeks.”
Steps for Families
- Teach the Pattern
- Example: “Here’s the pattern we often see in dementia.”
- Two-Week Forecast: “She seems steady, but these small changes are expected to continue without improvement.”
- Sample Family Forecast
- Explain: “Your loved one may have good and bad days.”
- Prepare: “Over time, bad days may increase, and recovery may be harder.”
- Reassure: “We’ll stay close and offer help for shortness of breath, like a comfort kit, if needed.”
- Respect Family Beliefs
- Ask: “How do you talk about serious illness in your family?”
- Adjust: “We’re planning for comfort as her body slows.” to respect cultural norms.
Closing Reflection
Patients do not decline in straight lines. But when you recognize the shape of likely decline, you can ready the road ahead. You can’t stop what’s coming, but you can guide patients and families through it.
As a new hospice physician, you don’t predict death’s arrival—you name the shape it takes and give guidance. That’s your work now, and your IDG team will help you refine it.
Three Key Insights
- “Unexpected” hospice deaths often reflect system failures, not clinical error.
- Recognizing trajectory patterns helps you plan, forecast, and communicate effectively.
- Preparation reshapes grief: when families know what’s possible, they suffer less shock.
Two Actionable Ideas
- Use the Two-Minute Forecast in IDG to normalize unpredictability and reduce panic.
- Name each patient’s illness trajectory in IDG to guide visit strategy and family education.
One Compassionate Call to Action
Don’t wait for surprise. Speak clearly. Speak early. Speak often. Trajectory recognition equips you and steadies families. Lean on your IDG’s seasoned nurses or social workers to refine your skills.
Share your story: Do you have tips for understanding illness trajectories as a new physician? Comment below or tag us on Instagram and Facebook (@HospiceSynopsis) to join the conversation.
Contact us: Discuss trajectory challenges and we can grow our skills together.
Glossary Terms
Trajectory of Decline: A pattern of decline commonly seen in patients with terminal illness. Hospice care uses four primary trajectories: Sudden Death, Terminal Illness, Organ Failure, and Frailty. Recognizing a patient’s trajectory guides clinical decisions, caregiver education, and resource planning.
Trajectory Mapping: The deliberate process of identifying and documenting the expected pattern of decline in a hospice patient, based on clinical observations and disease course. Used in IDG, charting, and caregiver teaching. Useful for Forecast Scripting.
Surprise Question: A prognostic tool from the UK’s Gold Standards Framework: “Would you be surprised if this patient were still alive in 12 months?” Used to trigger early palliative planning.
Six-Month Question: A formal inquiry guiding hospice eligibility: “Is the patient likely to live six months or less?” Requires clinical judgment—not certainty—but frames hospice certification decisions.
Sparks
“You can’t predict death’s timing, but naming its shape guides your care. #TrajectoryMatters”
“Miss the pattern, and grief surprises families. Name it, and your IDG aligns care. #HospiceMedEd”
“Trajectories are your roadmap to proactive hospice care. Start mapping today. #IDGReady”
“Don’t chase ‘when.’ Focus on ‘what’ to prepare patients and families. #PrognosisIsCare”
“How do you use trajectories to orient families? Share your tips! #HospiceTips”
Bibliography
Lunney JR, Lynn J, Hogan C. Patterns of functional decline at the end of life. JAMA. 2003;289(18):2387–2392. doi:10.1001/jama.289.18.2387
Lynn J, Adamson DM. Living Well at the End of Life: Adapting Health Care to Serious Chronic Illness in Old Age. RAND Corporation; 2003
FAQ: Common Questions Regarding Trajectory
Q: How do I know which trajectory my patient is on?
A: Ask in IDG for your teammates to describe the patient’s illness pattern, like stable periods or frequent crises. Use tools like the Palliative Performance Scale or others to clarify function patterns and discuss at IDG meetings.
Q: What should I ask my IDG to improve my trajectory recognition?
A: Ask, “What patterns have you seen in similar patients?” and “How can we adjust our care plan for this trajectory?” This leverages team expertise to guide decisions. Then care plan your changes.
Q: Can a patient’s trajectory change?
A: Yes, events like infections or injuries can shift a patient’s trajectory. Reassess and update the care plan with your IDG after major changes.
Leave a Reply